Life-course vaccination: for today, not tomorrow
Thinking about how to be a healthy older person is like thinking about glaciers crashing into Arctic seas as a result of climate change. Too far away to imagine, and we’ll worry when the effects reach our doorsteps. In reality, the challenge is here today asking all of us, at any age, to look ahead in order to have the highest possible positive impact on our communities and our own lives.
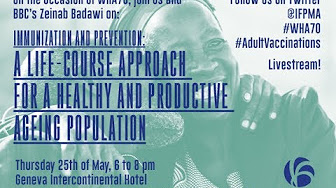
A life-course approach to vaccination is a major part of the solution to that challenge: how to be healthy as we age, and crucially, not to wonder how to be healthy only once we become ‘old’. As the World Health Assembly kicked off in Geneva last week, IFPMA convened a special panel of experts on the topic, and took a closer look at the benefits of not only preventing disease, but preventing decline, allowing all of us to grow older with greater energy and functionality.
Medical advances mean the global population is aging. By the year 2030, the percentage of the population that will be over 60 will outnumber children under five. By 2050, 80% of those older people will be living in developing countries. The pharmaceutical industry contributes to this longevity, and our work is a key part of maintaining quality of life throughout those years. Life-course vaccination means we are both better prepared to age healthily – free from disease and disability – as well as to enjoy those later years full of vitality.
A life-course approach to vaccination reduces disease burden: the measurable impact of health problems on quality of life, at any age. While the concept of healthy aging is widely used, it remains undefined and there are many, often complicated, indicators used to describe it. All essentially focus on functional ability, with the most common measure being ‘adjusted life years’ or the number of years lost due to disease. For example, infectious and parasitic diseases account for 37% of all years of potential life lost worldwide – an unhealthily large percentage and the single biggest category of all disease-burden categories. While we don’t yet know quite how to measure it, the potential for life- course vaccination to reduce disease burden is huge.
Nonetheless, there is a strong argument for the pharmaceutical industry to invest in developing vaccines and new formulations for older people, as immune system decline is an inevitable part of aging. Vaccines for older people relieve pressure on their carers and on healthcare systems, reduce the vulnerability of the community, and mean they can remain active members of society. An evidence-based approach helps us develop the right vaccines and vaccination policies for this segment of society. We know that up to 70% of seasonal flu-related hospitalizations, and up to 85% of seasonal flu-related deaths occur amongst those aged 65 and over. We also know that developed regions are not in any way exempt: those statistics come from the US, and people over 65 has been named one of the WHO priority target groups in Europe too due to its low influenza vaccine uptake rates. As a result, governments and advisory bodies worldwide make advice on influenza vaccines easily available not just for older people, but for everyone who may be part of their community.
The evidence-led approach is a clear win for public-health policy-makers. Vaccines are one of the most effective public health tools and investments for specific segments of the population, such as infants. However, the idea of life-course vaccination remains an underused, cost-effective public-health strategy, ultimately leading to long-term prosperity. Vaccinating people of all ages in a community has both social benefits – improving herd immunity – and economic benefits, as studies show that vaccines have the potential to save more adults than children. The mounting evidence in favor of life-course vaccinations shines a light on the gains to be made by preventing deaths of people at any age who could otherwise continue to be productive members of society.
Extending the benefits of vaccinations calls for a paradigm shift from multiple actors – from regulators to manufacturers to the patients themselves – in how we think about vaccinations and respond to changing demographics, i.e. not only to avoid disease, but to positively influence every individual’s functional capacity at any age. Life-course vaccination supports that shift. To change mindsets about the value of vaccination, we need systems and processes that support access and delivery. The role of industry here is to work with others to create the surveillance systems, process mass data, align healthcare systems to the needs of older people, design adequate vaccine response, and ensure widespread distribution. These are just some of the concrete actions that will be discussed at the WHA event by IFPMA and others.
WHO’s Global Strategy and Action Plan on Healthy Aging calls for a Decade of Healthy Aging from 2020-2030. How prevalent is the idea of life-course vaccination and prevention in that plan and what can IFPMA and others do to advance it? Rather than wait for the glacier to crash into the sea of population explosion that we know is coming, it is clear that there is will and momentum for these conversations to happen now. Have a look at how the discussion unfolded last week.
Author